
Case Study
NHS Utilises Digital Mental Health to Reduce Waitlists From Primary Through To Secondary Care
Lincolnshire Partnership NHS Foundation Trust’s integration of digital mental health interventions has helped address waitlist management, reduce clinician time by 58% and improve patient satisfaction.
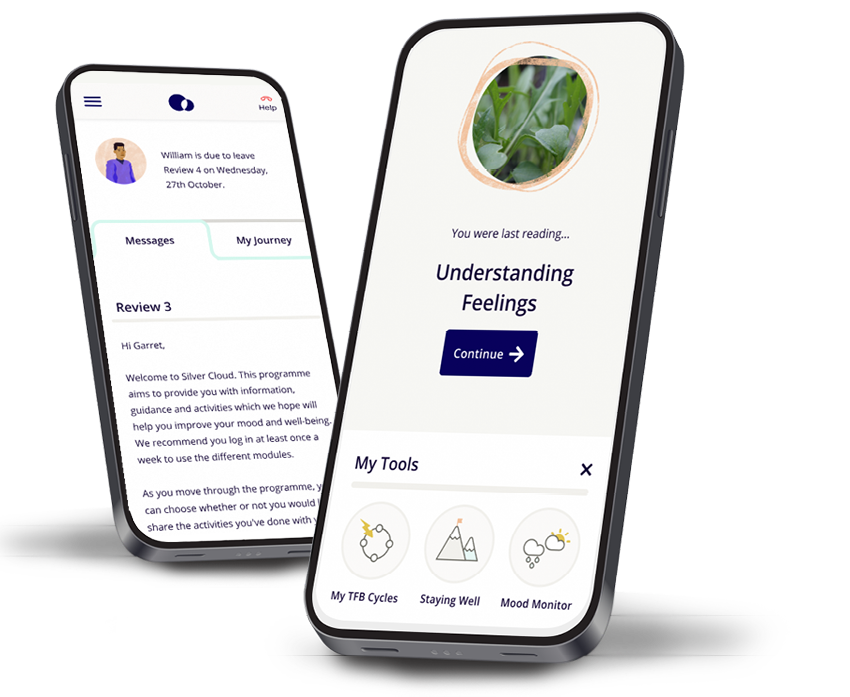
Lincolnshire Partnership NHS Foundation Trust (LPFT) partnered with SilverCloud® by Amwell® in 2018 to increase access to evidence-based digital mental health support to over 13,000 patients.
As an early adopter of digital mental health provision, LPFT has gained valuable insights into the patients and clinician benefits of integrating digital into care pathways in Talking Therapies (TT) and secondary care services.
Programmes
| Talking Therapies: | Secondary care: |
|
|

The Challenge
LPFT introduced the SilverCloud platform to its TT service in 2018. The goals were to help meet the increased demand for mental health services and to support equitable service delivery across a diverse and geographically dispersed population.
Central to the deployment of the SilverCloud® platform was the need to ensure digital services followed the NHS Talking Therapies (formerly IAPT) and NICE guidelines. “Offering digital can’t be about doing something. It’s essential that we do the right thing. It’s got to be a good fit for people,” says Claire Hancox, Service Manager of Lincolnshire NHS TT. Since its implementation, the SilverCloud platform showed 823% growth in activations and supported LPFT to deliver care more efficiently, flexibly and cost-effectively within its services. Following the success, the trust implemented the programmes at secondary care level, to support the delivery of mental health care.
As well as relieving pressure on services, the goals for this initiative included improving patient care and satisfaction, and supporting staff to deliver timely, high-quality evidence-based care. In addition, as the rollout of integrated primary and community mental health services continues, LPFT is exploring the potential for digital to support continuity and seamless transitions between services.
The Approach
Activations, Engagement and Completions
Right from the outset, Lincolnshire TT achieved impressive results with 96% of SilverCloud accounts activated. The trust sits in the top tier of NHS Talking Therapies services using SilverCloud programmes.
Engagement figures are equally impressive with 50% of users on supported programmes logging in an average of 32 times and 45% of users engaging with the programme content for an average total of 6.7 hours. Programme completion rates are 20% above the national average.

Resource Efficiencies
Lincolnshire Talking Therapies found that supporting a patient on a SilverCloud programme reduces the time spent by clinicians by 58% compared to a typical face-to-face treatment whilst helping the patient to achieve the dose of treatment that is right for them. In the digital pathway, patients are spending more time engaging with therapeutic content -- an average of 4 hours and 12 minutes - compared face-to-face treatment, which averages 3 hours.
These shorter contacts mean that Psychological Wellbeing Practitioners (PWPs) can increase their caseload without becoming overwhelmed.

"We’re very firmly of the belief that the diagnosis (which LPFT always align to an ICD-10 code), the treatment package and the patient goals need to match. Those three things form a triangle that give you the best engagement and the best treatment outcomes. We’ve worked hard on the content of the review emails. They are encouraging and positive and instil hope that people can get better."
Claire Hancox, Service Manager of Lincolnshire NHS TT

“It adds variety as well. It’s that mixture of delivering different types of treatment that keeps the role varied.”
Claire Hancox, Service Manager of Lincolnshire NHS TT
High Patient Satisfaction
Given the strong engagement rates, it’s perhaps not surprising that overall patient satisfaction is very positive. At the end of each module, SilverCloud users are prompted to rate the section they have just completed. The overall satisfaction rate is 94% for supported programmes with the majority of patients saying they agree or strongly agree that the module was interesting (95%), relevant (95%), helpful (93%) and helping them make progress (93%).
Digital Waitlist Management in Talking Therapies: The Self-Management Toolkit
LPFT TT introduced SilverCloud’s Self-Management Toolkit in August 2023 to support patients waiting for treatment. This self-help style programme provides patients with psychoeducation and CBT skills and tools. Activated accounts have risen steadily month-on-month with an average increase of 18%. Users of the programme are not supported by a clinician and satisfaction rates are very high (83% ) Although it’s still early, the programme has seen growth of 394% since implementation and Claire Hancox is optimistic that the programme will have a positive impact on patient outcomes.

"We’re hoping that people who use the programme will be more ready for therapy when they do get to the top of the list. That might be because they are more psychologically minded or will perhaps have engaged with some of the initiatives on the programme already and be feeling slightly better."
Claire Hancox, Service Manager of Lincolnshire NHS TT
Engagement measures for SilverCloud programmes within Lincolnshire Talking Therapies
-
94% patient satisfaction for supported programmes1
-
96% accounts activated
-
20% higher completion rates than national average
-
58% reduction in clinician time2
94% patient satisfaction for supported programmes1
96% accounts activated
20% higher completion rates than national average
58% reduction in clinician time2
1. Data from the SilverCloud dashboard
2. Versus average face-to-face treatment

The Promising Transition to Secondary Care
Recognising the difference the SilverCloud platform has made to TT, LPFT is now exploring its use within secondary care.
With secondary care patients having more complex needs than those treated by Talking there is no doubt that this process has some challenges. But Steve Skinner, Service Development Lead at LPFT Adult Community Division, is confident that with the right implementation, there are benefits to the patients and staff within his service.

"The way in which we're delivering the intervention is different in secondary care,” Skinner explains. “We've got a group of patients who are more complex than in a Talking Therapies service who often require multi-professional care and support plans. This means pure remote working isn't such a good or safe option. Instead, we’re introducing the digital products alongside regular face-to-face contacts as an integrated part of our offer. It’s fully embedded in what we do. "
Steve Skinner, Service Development Lead at LPFT Adult Community Division
Amwell has supported the expansion of digital therapeutics into secondary care by partnering with services, including LPFT, to develop tools and programmes specifically intended for use among community mental health teams. For example, the Recoveryprogramme is designed for adults with a range of long-term mental health concerns such as depression, anxiety, post-traumatic stress disorder and psychotic illnesses. “It was essential to us that the digital offer be relevant to secondary care presentations and flexible enough to be tailored to a patient’s needs,” says Skinner. Since implementing the Recovery programme, LPFT has seen an increase in usage, with activations increasing monthly, and 92% user satisfaction rate.
Preparing for Treatment
Right from the point of referral, the Recovery programme can be offered to patients, where appropriate, to help them prepare for therapy. “It's really good for us in getting people to think about what goals they want out of therapy,” says Skinner. “Plus, it provides some really good stabilisation tools right at the front of their journey.”
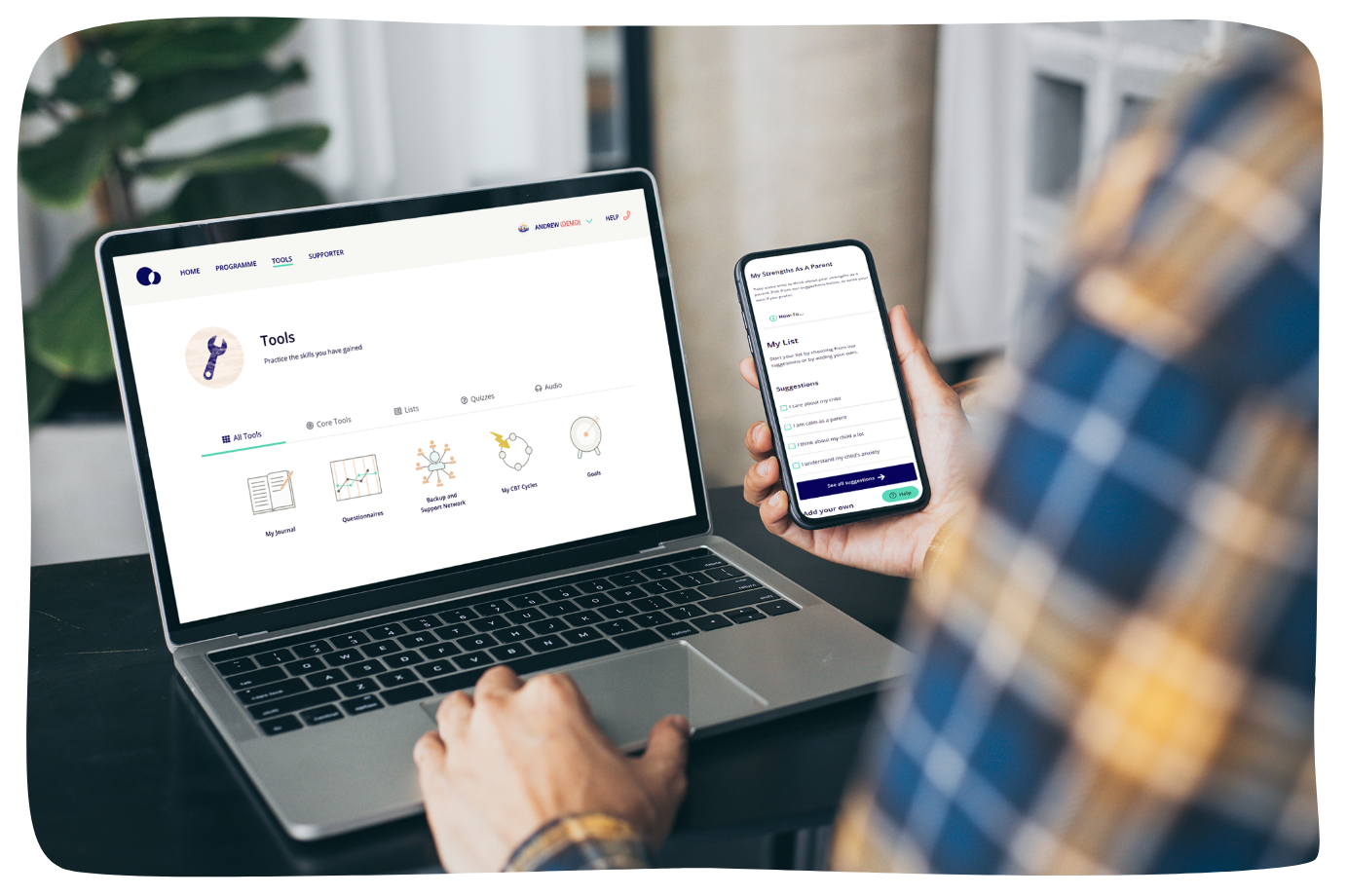
Moving Practice Forwards
The content in SilverCloud’s programmes is evidence-based and aligned to NICE guidelines, so clinicians are supported to use methods and approaches that meet current standards. Unlike paper-based work, which is easy to lose, patients can access the tools and their work at any time from any computer or mobile device. That’s a huge benefit, says Skinner. “Sometimes a piece of work might not feel so relevant to a patient when they first encounter it, but because they've got access to it over the longer space of time, they can go back to those bits of information and use it as they need to.”
Supporting the Integrated Care Transformation
“The transformation agenda is about trying to remove barriers between primary care and secondary care and ensuring there are no cliff edges in terms of people not dropping off from having high levels of support to suddenly being back with their GP,” explains Skinner. The SilverCloud platform is supporting this key initiative by providing ongoing access to programmes even after treatment has ended. “There is a strong case to use digital as a support to relapse prevention,” he says.
LPFT has also developed new roles under the Additional Roles Reimbursement Scheme (ARRS), such as the Psychological Interventions Facilitators (PIF) and Mental Health and Wellbeing Practitioners (MHWP), to deliver low-intensity interventions in secondary care. Using SilverCloud programmes for these interventions ensures a consistency in the messaging throughout an integrated primary community mental health service.
Positive User Feedback
Early results from user feedback show the majority of SilverCloud users in secondary care agree or strongly agree that the modules are
-
interesting 93%
-
relevant 98%
-
helpful 90%%
-
helping them make progress 86%
interesting 93%
relevant 98%
helpful 90%%
helping them make progress 86%
What’s Next for LPFT?
The challenge now is to develop the evidence base for digital products in secondary care. As more data becomes available, LPFT, in partnership with Amwell, hopes to prove that these tools can enhance efficiency, provide data-driven insights and facilitate better decision making, all while preserving the essential skills and empathy that therapists bring to their practice. Looking to the future, the clinical team in Lincolnshire envisions a digital passport concept, where individuals can adapt their digital tools to meet their changing needs as they progress through an integrated care service.
Book a demo
References
-
- https://www.england.nhs.uk/mental-health/taskforce/imp/mh-dashboard/
- Gov.UK (2022). https://www.gov.uk/government/publications/a-plan-for-digital-health-and-social-care/a-plan-for-digital-health-and-social-care.
- Richards, D., Enrique, A., et al. (2020). NPJ Digital Medicine 3, 85.
- Richards, D., Murphy, T., et al. (2016). Internet Interventions 5, 12-22.
- Duffy, D., Enrique, A., et al. (2020). Frontiers in psychiatry 10, 902.
- National Institute for Health and Care Excellence (NICE) (2022). www.nice.org.uk/process/pmg36/chapter/economic-evaluation.
- HM Treasury (2022). www.gov.uk/government/publications/the-green-book-appraisal-and-evaluation-in-central-governent/the-green-book-2020.
- National Institute for Health and Care Excellence (NICE) (2020). https://www.nice.org.uk/advice/mib215.
- https://www.pssru.ac.uk/unitcostsreport/










